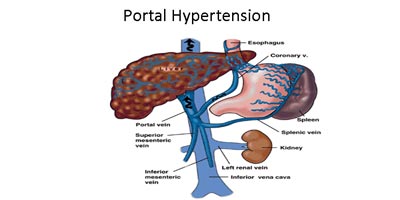
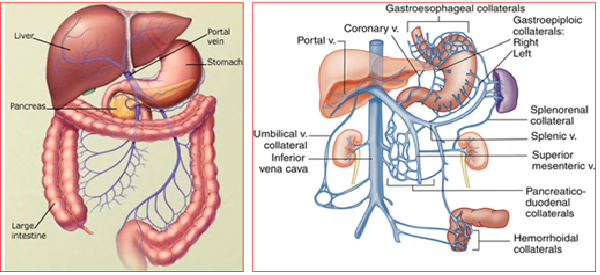
Portal hypertension is a high blood pressure in the portal blood system which is the portal vein and its branches, which drain from most of the intestines to the liver. If the vessels in the liver are blocked, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein over a time may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button). Varices can rupture and bleed, resulting in potentially life-threatening complications.
The blockage of blood vessels can happen at any of three places. One, Pre-hepatic i.e blockage of portal vein before it enters into the liver. Second, blockage inside the liver and Third, post-hepatic, blockage of blood vessels (hepatic veins) outside the liver. There are different causes of blockage at all three levels.
The most common cause of portal hypertension is cirrhosis of the liver. Cirrhosis is a condition in which the liver slowly deteriorates and is unable to function normally due to chronic, or long lasting, injury. Scar tissue replaces healthy liver tissue and partially blocks the flow of blood through the liver.
Other causes of portal hypertension include blood clots in the portal vein, blockages of the veins that carry the blood from the liver to the heart, a parasitic infection called schistosomiasis. Sometimes the cause is unknown despite all investigations.
Symptoms of portal hypertension are non-specific. Vague abdominal discomfort is common but non-specific. Usually portal hypertension is diagnosed when it progress to its complications. In vast majority of the cases, one of the complications may be the first clue about it. The main symptoms and complications of portal hypertension include:
Based on symptoms, blood test, Sonography with Doppler study & Endoscopy is usually required to make diagnosis.
Bleeding from gastric or oesophageal varices – the most common complication of portal hypertension. Gastric varices occur in around 20% of patients with portal hypertension, mostly secondary to liver cirrhosis.
Infection (Spontaneous bacterial peritonitis)
Hepatorenal syndrome (a complication of cirrhosis with ascites)
Fluid in Lung (Hepatic hydrothorax)
Porto-pulmonary hypertension (pulmonary arterial hypertension complicating portal hypertension in patients with liver disease). Hepatopulmonary syndrome (a triad of hepatic dysfunction, hypoxaemia and extreme vasodilation in the form of intrapulmonary vascular dilations).
The portal hypertension itself is difficult to treat effectively, except by treating the underlying cause (where possible) and liver transplantation (if indicated and feasible).
Portal venous pressure can be reduced by medicine (beta-blockers ± nitrates) and by using surgery (shunt procedures) to create an new joint ( anastomosis) between the portal systemic veins.
- Beta-blockers: Non-selective beta-blockers reduce portal pressure in many patients. They reduce rates of bleeding and re-bleeding in patients with oesophageal varices.
- Nitrates: Added to beta-blocker therapy, they contribute to reducing portal pressure and may reduce rates of variceal re-bleeding.
- Vasoactive drugs: Terlipressin and octreotide are used to assist the control of acute variceal bleeding.
- Endoscopy – to detect and monitor oesophageal varices.
- Endoscopic vein ligation – to prevent bleeding of oesophageal varices.
- For gastric varices with acute bleeding, endoscopic variceal obturation with tissue adhesives (eg, cyanoacrylate) is effective – but there are recognised complications (mucosal ulceration and thromboembolism).
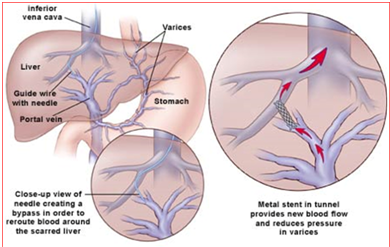
This is a radiological procedure, connecting the portal and hepatic veins using a stent. The purpose of a TIPS is to decompress the portal venous system, to prevent re-bleeding from varices or to reduce the formation of ascites. However, there are potential complications – hepatic encephalopathy and deteriorating liver function. The stent may stenose; it requires follow-up and may require repeat procedures.
Surgical porto-systemic shunts:
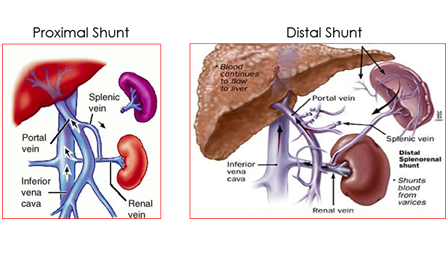
- These require major surgery and an experienced surgeon. They are less likely to stenose than TIPS and can be used where TIPS is not feasible.
- Shunts may be total, partial or selective.
- Include gastro-oesophageal devascularisation, splenectomy and oesophageal transection.
- Generally used where other therapies are unsuitable.
To book your appointment with a gastro surgeon, please reach out to us on +91 8160650099

