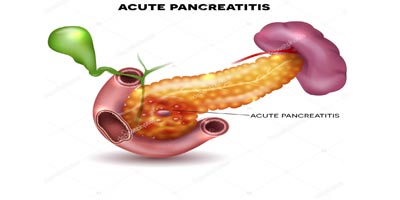
It is an acute inflammation of the pancreas,where the pancreas becomes swollen and leaks its juices.Acute Pancreatitis may be mild, moderate or severe.
Most of the patient develop mild pancreatitis(80%). Mild pancreatitis is a self remitting disease and most of the patients are better within few days with supportive treatment though they require hospitalization.
Moderate and severe type of pancreatitis take long time for recovery sometime may upto months. Those patients who develop complications related to pancreatitis need to be managed in specialized centre. Even in best of the centres around the world, severe pancreatitis patient can succumb to it.
Common Causes:
Symptoms:
Based on the typical history of upper abdominal pain radiating to the back the diagnosis of acute pancreatitis is suspected. Presence of high blood amylase or lipase or imaging (ultrasound/CT/MRI) will clinch the diagnosis. All tests are not required to diagnose acute pancreatitis, presence of two of the three things ( history, amylase/lipase or imaging) is enough to diagnose this condition.
Any patient diagnosed to have acute pancreatitis should be treated in a specalist center experienced in managing these cases. These patients are initially admitted in intensive care for monitoring and treatment. Initial treatment consists of intravenous fluid administration, painkillers and sometimes oxygen support. Mild acute pancreatitis usually resolves with these simple measures within a week. Patients are monitored for pulse, blood pressure, urine output, blood oxygen levels in the ICU. If they improve they are shifted to the ward in cases of mild attacks.
Some patients develop more severe form of pancreatitis and requires prolonged ICU stay. Their pancreas may become necrotic or dead, partly or wholly and may get infected. They may develop collection of fluid, pus or necrotic material inside abdomen. Some patients may develop organ failure (kidney, heart or respiratory failure).
Ultrasound and liver function test are always done initially to rule out gallbladder stone as the cause of pancreatitis. If gallbladder stone is found to be blocking bile duct or causing fever with chills it needs to be cleared with ERCP (Endoscopic Retrograde Cholangiopancreatography); an endoscopic method of bile duct stone removal.
Treatment is like mild cases, but may continue for a longer duration. When they develop infection antibiotics may be required to treat that. This usually ocuurs in the 3rd or 4th week of disease. Clear fluid collections (acute peripancreatic fluid collection) in the early stages of the disease usually resolves spontaneously and do not require any drainage. When they develop wall around the collection (Pseudocyst) they may be left alone if asymptomatic or may be drained internally by endoscopic or laparoscopic/open surgical method if they develop pain abdomen or vomiting.
When the pancreas is necrotic, initially these patients will develop acute necrotic collection and later on walled off pancreatic necrosis. These will require some form of drainage if they are not improving with medical treatment. Drainage is initially by percutaneous means, if this technique fails surgical removal (necrosectomy) is necessary. Surgery gives best result if it is done after 4 weeks.
In all cases of acute pancreatitis patients are allowed normal diet as soon as possible , otherwise a tube is placed in the stomach or jejunum and fed through that.
Where there is organ failure, ventilator support for lungs or dialysis for kidney may be required.
Contrast enhanced CT or MRI may be required in severe cases to confirm necrosis and to plan interventions (percutaneous or surgical drainage). This may need to be repeated depending the clinical course of the patient.
To book your appointment with a gastro surgeon, please reach out to us on +91 8160650099

