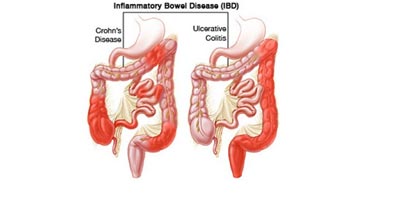
Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of your digestive tract. IBD primarily includes ulcerative colitis and Crohn’s disease. IBD can be painful and debilitating, and sometimes leads to life-threatening complications.
Ulcerative colitis is an inflammatory bowel disease that causes long-lasting inflammation in part of your digestive tract. Symptoms usually develop over time, rather than suddenly. Ulcerative colitis usually affects only the innermost lining of your large intestine (colon) and rectum. It occurs only through continuous stretches of your colon.
Crohn’s disease is an inflammatory bowel disease that causes inflammation anywhere along the lining of your digestive tract, and often spreads deep into affected tissues. This can lead to abdominal pain, severe diarrhea and even malnutrition. The inflammation caused by Crohn’s disease can involve different areas of the digestive tract in different people.
Inflammatory bowel disease symptoms vary, depending on the severity of inflammation and where it occurs.
Ulcerative colitis is classified according to its signs and symptoms:
The course of ulcerative colitis varies, with periods of acute illness often alternating with periods of remission. Most people with a milder condition, such as ulcerative proctitis, won’t go on to develop more-severe signs and symptoms.
Inflammation of Crohn’s disease may involve different parts of the digestive tract in different people. The most common areas affected by Crohn’s disease are the last part of the small intestine called the ileum and the colon. Inflammation may be confined to the bowel wall, which can lead to scarring (stenosis), or inflammation may spread through the bowel wall (fistula).
Signs and symptoms of Crohn’s disease can range from mild to severe and may develop gradually or come on suddenly, without warning. Signs and symptoms may include:
People with severe Crohn’s disease may also experience:
No one is quite sure what triggers inflammatory bowel disease, but there’s a consensus as to what doesn’t. Researchers no longer believe that diet and stress are main causes, although stress can often aggravate symptoms. Instead, current thinking focuses on the:
Inflammatory bowel disease affects about the same number of women and men. Risk factors may include:
Inflammatory bowel disease may lead to one or more of the following complications:
Your doctor will likely diagnose inflammatory bowel disease only after ruling out other possible causes for your signs and symptoms, including ischemic colitis, infection, irritable bowel syndrome (IBS), diverticulitis and colon cancer. To help confirm a diagnosis of IBD, you may have one or more of the following tests and procedures:
The goal of inflammatory bowel disease treatment is to reduce the inflammation that triggers your signs and symptoms. In the best cases, this may lead not only to symptom relief but also to long-term remission. IBD treatment usually involves either drug therapy or surgery.
Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. That includes Mesalamine.
These drugs also reduce inflammation, but they target your immune system rather than treating inflammation itself. Because immune suppressors can be effective in treating ulcerative colitis, scientists theorize that damage to digestive tissues is caused by your body’s immune response to an invading virus or bacterium or even to your own tissue. By suppressing this response, inflammation is also reduced. Immune system suppressors are associated with a small risk of developing cancer, such as lymphoma. Immunosuppressant drugs includes, Azathioprine and Infliximab . This drug is specifically for those with moderate to severe ulcerative colitis who don’t respond to or can’t tolerate other treatments. It works quickly to bring on remission, especially for people who haven’t responded well to corticosteroids. It works by neutralizing a protein produced by your immune system known as tumor necrosis factor (TNF).
Some people with heart failure, people with multiple sclerosis, and people with cancer or a history of cancer can’t take infliximab. The drug has been linked to an increased risk of infection, especially tuberculosis and reactivation of viral hepatitis, and may increase your risk of blood problems and cancer. You’ll need to have a skin test for tuberculosis, a chest X-ray and a test for hepatitis B before taking infliximab. That includes, Adalimumab and Methotrexate.
Antibiotics can reduce the amount of drainage and sometimes heal fistulas and abscesses in people with Crohn’s disease. Researchers also believe antibiotics help reduce harmful intestinal bacteria and suppress the intestine’s immune system, which can trigger symptoms. However, there’s no strong evidence that antibiotics are effective for Crohn’s disease. Frequently prescribed antibiotics includes, Metronidazole and Ciprofloxacin.
In addition to controlling inflammation, some medications may help relieve your signs and symptoms. Depending on the severity of your inflammatory bowel disease, your doctor may recommend one or more of the following: Anti-diarrheals, Laxatives, Pain relievers, Iron supplements, B-12 shots, Calcium and vitamin D supplements.
If diet and lifestyle changes, drug therapy, or other treatments don’t relieve your IBD signs and symptoms, your doctor may recommend surgery.
People who have inflammatory bowel disease have an increased risk of colon cancer. Talk with your doctor about how often you should be screened.
There’s no firm evidence that what you eat causes inflammatory bowel disease. But certain foods and beverages can aggravate your symptoms, especially during a flare-up. It’s a good idea to try eliminating from your diet anything that seems to make your signs and symptoms worse. Here are some suggestions:
Smoking increases your risk of developing Crohn’s disease, and once you have it, smoking can make the condition worse. People with Crohn’s disease who smoke are more likely to have relapses, need medications and repeat surgeries. Quitting smoking can improve the overall health of your digestive tract, as well as provide many other health benefits.
Although stress doesn’t cause inflammatory bowel disease, it can make your signs and symptoms much worse and may trigger flare-ups.
To book your appointment with a gastro surgeon, please reach out to us on +91 8160650099

