An anal fissure is a small tear in the thin, moist tissue (mucosa) that lines the anus. An anal fissure may occur when you pass hard or large stools during a bowel movement. Anal fissures typically cause pain and bleeding with bowel movements. You also may experience spasms in the ring of muscle at the end of your anus (anal sphincter).
Anal fissures are very common in young infants but can affect people of any age. An anal fissure usually heals on its own within four to six weeks. If it doesn’t, medical treatment or surgery usually can relieve discomfort.
Factors that may increase your risk of developing an anal fissure include:
Complications of anal fissure can include:
Your doctor will likely ask about your medical history and perform a physical exam, including inspection of the anal region. Often the tear is visible. Usually this exam is all that’s needed to diagnose an anal fissure.
Your doctor will probably refrain from performing a digital rectal exam, which involves inserting a gloved finger into your anal canal, because it is likely to be too painful. If anal fissure is suspected but can’t be identified, your doctor may use a short, lighted tube (anoscope) to inspect your anal canal.
The fissure’s location offers clues about its cause. A fissure that occurs on the side of the anal opening, rather than the back or front, is more likely to be a sign of another disorder, such as Crohn’s disease. If an underlying condition is suspected, your doctor may recommend further testing:
Flexible sigmoidoscopy. A thin, flexible tube with a tiny video camera is inserted into the bottom portion of your colon. This test may be done if you’re younger than 50 and have no risk factors for intestinal diseases or colon cancer.
Colonoscopy. A flexible tube is inserted into your rectum to inspect the entire colon. This test may be done if you are older than age 50 or have risk factors for colon cancer, signs of other conditions, or other symptoms such as abdominal pain or diarrhea.
Anal fissures often heal within a few weeks if you take steps to keep your stool soft, such as increasing your intake of fiber and fluids. Soaking in warm water for 10 to 20 minutes several times a day, especially after bowel movements, can help relax the sphincter and promote healing.
If your symptoms persist, you’ll likely need further treatment.
Your doctor may recommend:
Externally applied nitroglycerin, to help increase blood flow to the fissure and promote healing, and to help relax the anal sphincter. Nitroglycerin is generally considered the medical treatment of choice when other conservative measures fail. Side effects may include headache.
Botulin toxin type A (Botox) injection, to paralyze the anal sphincter muscle and relax spasms.
Blood pressure medications, which can help relax the anal sphincter. These medications may be taken by mouth or applied externally and may be used when nitroglycerin in not effective or causes significant side effects.
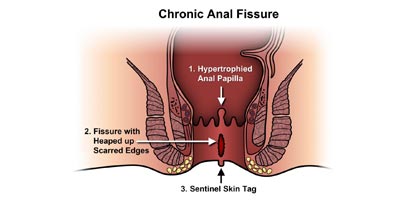
If you have a chronic anal fissure that is resistant to other treatments, or if your symptoms are severe, your doctor may recommend surgery. Surgery usually involves cutting a small portion of the anal sphincter muscle to reduce spasm and pain and promote healing. Surgery has a small risk of causing incontinence.
Several lifestyle changes may help relieve discomfort and promote healing of an anal fissure, as well as prevent recurrences:
If your infant has an anal fissure, be sure to change diapers frequently, wash the area gently and discuss the problem with your infant’s doctor.
You may be able to prevent an anal fissure by taking measures to prevent constipation. Eat high-fiber foods, drink fluids and exercise regularly to keep from having to strain during bowel movements.
To book your appointment with a gastro surgeon, please reach out to us on +91 8160650099

