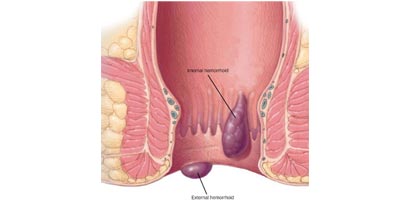
Hemorrhoids (HEM-uh-roids), also called piles, are swollen and inflamed veins in your anus and lower rectum. Hemorrhoids may result from straining during bowel movements or from the increased pressure on these veins during pregnancy, among other causes. Hemorrhoids may be located inside the rectum (internal hemorrhoids), or they may develop under the skin around the anus (external hemorrhoids).
Hemorrhoids are common ailments. By age 50, about half of adults have had to deal with the itching, discomfort and bleeding that can signal the presence of hemorrhoids.
Fortunately, many effective options are available to treat hemorrhoids. Most people can get relief from symptoms by using home treatments and making lifestyle changes.
Signs and symptoms of hemorrhoids may include:
Hemorrhoid symptoms usually depend on the location. Internal hemorrhoids lie inside the rectum. You usually can’t see or feel these hemorrhoids, and they usually don’t cause discomfort.
But straining or irritation when passing stool can damage a hemorrhoid’s delicate surface and cause it to bleed. Occasionally, straining can push an internal hemorrhoid through the anal opening. This is known as a protruding or prolapsed hemorrhoid and can cause pain and irritation.
External hemorrhoids are under the skin around your anus. When irritated, external hemorrhoids can itch or bleed. Sometimes blood may pool in an external hemorrhoid and form a clot (thrombus), resulting in severe pain, swelling and inflammation.
The veins around your anus tend to stretch under pressure and may bulge or swell. Swollen veins (hemorrhoids) can develop from an increase in pressure in the lower rectum. Factors that might cause increased pressure include:
Hemorrhoids are more likely as you get older because the tissues that support the veins in your rectum and anus can weaken and stretch with aging.
Complications of hemorrhoids are rare but include:
Your doctor may be able to see if you have external hemorrhoids simply by looking. Tests and procedures to diagnose internal hemorrhoids may include:
Your doctor may want to do a more extensive examination of your entire colon using colonoscopy. This might be recommended if:
Most of the time, treatment for hemorrhoids involves steps that you can take on your own, such as lifestyle modifications. But sometimes medications or surgical procedures are necessary.
If a blood clot has formed within an external hemorrhoid, your doctor can remove the clot with a simple incision, which may provide prompt relief.
For persistent bleeding or painful hemorrhoids, your doctor may recommend another minimally invasive procedure. These treatments can be done in your doctor’s office or other outpatient setting.
Hemorrhoid banding can be uncomfortable and may cause bleeding, which might begin two to four days after the procedure but is rarely severe.
If other procedures haven’t been successful or you have large hemorrhoids, your doctor may recommend a surgical procedure. Surgery can be performed on an outpatient basis or you may need to stay in the hospital overnight.
Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications may include temporary difficulty emptying your bladder and urinary tract infections associated with this problem.
Most people experience some pain after the procedure. Medications can relieve your pain. Soaking in a warm bath also may help.
The best way to prevent hemorrhoids is to keep your stools soft, so they pass easily. To prevent hemorrhoids and reduce symptoms of hemorrhoids, follow these tips:
To book your appointment with a gastro surgeon, please reach out to us on +91 8160650099

