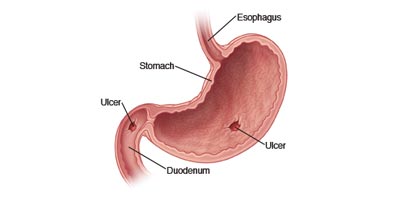
Peptic ulcers are open sores that develop on the inside lining of your esophagus, stomach and the upper portion of your small intestine. The most common symptom of a peptic ulcer is abdominal pain.
Peptic Ulcers Include:
Symptoms:
Other Signs Or Symptoms:
Risk Factors:
Complications
In order to detect an ulcer, you may have to undergo diagnostic tests, such as:
During endoscopy, your doctor passes a hollow tube equipped with a lens (endoscope) down your throat and into your esophagus, stomach and small intestine. Using the endoscope, your doctor looks for ulcers.
If your doctor detects an ulcer, small tissue samples (biopsy) may be removed for examination in a lab. A biopsy can also identify the presence of H. pylori in your stomach lining.
Your doctor is more likely to recommend endoscopy if you are older, have signs of bleeding, or have experienced recent weight loss or difficulty eating and swallowing.
Sometimes called a barium swallow or upper gastrointestinal series, this series of X-rays creates images of your esophagus, stomach and small intestine. During the X-ray, you swallow a white liquid (containing barium) that coats your digestive tract and makes an ulcer more visible.
Treatment for peptic ulcers is often successful, leading to ulcer healing. But if your symptoms are severe or if they continue despite treatment, your doctor may recommend endoscopy to rule out other possible causes for your symptoms.
If an ulcer is detected during endoscopy, your doctor may recommend another endoscopy after your treatment to make sure your ulcer has healed. Ask your doctor whether you should undergo follow-up tests after your treatment.
Peptic ulcers that don’t heal with treatment are called refractory ulcers. There are many reasons why an ulcer may fail to heal. These reasons may include:
Less often, refractory ulcers may be a result of:
To book your appointment with a gastro surgeon, please reach out to us on +91 8160650099

